Acute gastroenteritis is a common and often unpleasant condition that affects millions of people worldwide each year. It is inflammation of the stomach and intestines that typically results in diarrhea, vomiting, and abdominal pain. Although it usually resolves on its own, understanding its causes, symptoms, and prevention strategies can help you effectively manage and avoid this condition.
- What is acute gastroenteritis?
- Causes
- Symptoms
- Diagnosis
- Treatment
- 1. Hydration and Electrolyte Replacement
- 2. Dietary Management
- 3. Medication
- 4. Rest and Recovery
- 5. Monitoring and Follow-Up
- 6. Preventive Measures
- Initial Phase: Rest and Rehydration
- Transition Phase: Introducing Solid Foods
- Gradual Reintroduction of Normal Foods
- Foods and Drinks to Avoid
- Sample Meal Plan for Acute Gastroenteritis
- Prevention
- When to seek medical help
- Conclusion
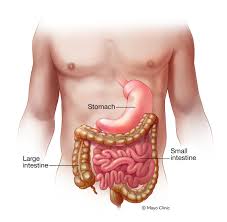
What is acute gastroenteritis?
Acute gastroenteritis is characterized by the sudden onset of inflammation in the gastrointestinal (GI) tract, which includes the stomach and intestines. This condition is commonly known as the “stomach flu,” although it is not caused by the influenza virus. Instead, it is typically caused by a number of infectious agents, including viruses, bacteria, and parasites.
Causes
- Virus: The most common cause of acute gastroenteritis is a viral infection. Norovirus and rotavirus are the main causes. Norovirus, in particular, is notorious for causing outbreaks in close-knit communities, such as schools and cruise ships.
- Bacteria: Bacterial infections, such as those caused by Salmonella, E. coli, and Campylobacter, can cause gastroenteritis. These infections are often associated with contaminated food or water.
- Parasites: Although less common, parasites such as Giardia and Cryptosporidium can also cause gastroenteritis. These are often transmitted through contaminated water.
- Toxins: Sometimes, toxins produced by bacteria (e.g., Staphylococcus aureus or Clostridium perfringens) can lead to symptoms of gastroenteritis. This is often associated with eating contaminated or improperly stored food.
Symptoms
The symptoms of acute gastroenteritis can range from mild to severe and typically include:
- Diarrhea: Frequent, watery stools are a prominent symptom.
- Vomiting: This often accompanies diarrhea and can be severe.
- Abdominal pain: Cramping and discomfort in the abdominal area are common.
- Fever: Mild fever may be accompanied by other symptoms.
- Nausea: A persistent feeling of nausea is common.
Symptoms typically appear within one to three days of exposure to the infectious agent and may last from a few days to a week.
Diagnosis
The diagnosis is usually based on the patient’s symptoms and medical history. In severe or long-standing cases, stool samples may be tested to identify the specific pathogen causing the illness. Blood tests may also be performed if there is concern about dehydration or more serious complications.
Treatment
Most cases of acute gastroenteritis resolve on their own with supportive care. Key aspects of treatment include:
1. Hydration and Electrolyte Replacement
Importance: Dehydration is a major concern in acute gastroenteritis due to the loss of fluids and electrolytes from vomiting and diarrhea.
Treatment:
- Oral Rehydration Solutions (ORS): These are specially formulated to replace lost fluids and electrolytes. They are often the first line of treatment and are preferred over plain water because they contain the right balance of salts and sugars. Popular ORS brands include Pedialyte and Ceralyte.
- Clear Broths: Chicken or vegetable broths can provide hydration and some nutrients. They are easier on the stomach and can help maintain fluid balance.
- Diluted Juices: Apple or pear juice, diluted with water, can help provide some calories and hydration but should be used in moderation due to potential sugar content.
Avoid:
- Caffeinated Beverages: Coffee, tea, and sodas can exacerbate dehydration.
- Alcohol: Can irritate the gastrointestinal tract and worsen dehydration.
- Sugary Drinks: Can increase diarrhea and are not effective for rehydration.
2. Dietary Management
Initial Phase:
- Start with Clear Liquids: Once you can keep fluids down, start with clear liquids to avoid further irritation of the gastrointestinal tract.
- Gradual Introduction of Bland Foods: After the initial phase, gradually introduce bland, easily digestible foods. The BRAT diet (bananas, rice, applesauce, toast) is a good starting point.
Transition to Normal Diet:
- Increase Fiber Gradually: Once symptoms improve, slowly reintroduce low-fiber foods. White rice, plain pasta, and soft-cooked vegetables are suitable choices.
- Lean Proteins: Include skinless chicken, turkey, and tofu. These are easier to digest and provide essential nutrients.
- Cooked Vegetables: Soft, well-cooked vegetables like carrots and spinach are gentle on the stomach.
Foods to Avoid:
- Dairy Products: Milk, cheese, and yogurt can be hard to digest and may worsen diarrhea, especially if you have temporary lactose intolerance.
- Fatty Foods: Avoid fried foods, rich sauces, and high-fat meats as they can irritate the digestive system.
- Spicy Foods: These can exacerbate symptoms and should be avoided until recovery is complete.
- High-Sugar Foods: Sweets and sugary snacks can lead to increased diarrhea and are best avoided.
3. Medication
Over-the-Counter Options:
- Anti-Diarrheal Medications: Loperamide (Imodium) can help reduce diarrhea but should be used with caution. It is generally not recommended for children and should be avoided if a bacterial infection is suspected.
- Anti-Nausea Medications: Medications like dimenhydrinate (Dramamine) or meclizine (Antivert) can help manage nausea and vomiting.
Consult Healthcare Providers:
- Antibiotics: Not typically required for viral gastroenteritis but may be necessary if a bacterial infection is confirmed. Common bacterial causes like Salmonella or E. coli may require specific antibiotic treatment.
- Antiparasitics: If a parasitic infection is diagnosed, antiparasitic medications will be prescribed.
4. Rest and Recovery
Importance: Resting allows your body to recover and helps your immune system combat the infection.
Recommendations:
- Get Plenty of Sleep: Adequate rest supports your body’s healing process and helps you recover more quickly.
- Avoid Strenuous Activities: Focus on light activities and rest until you feel fully recovered.
5. Monitoring and Follow-Up
When to Seek Medical Attention:
- Severe Dehydration: Signs include excessive thirst, dry mouth, reduced urine output, and dizziness.
- Persistent Symptoms: Symptoms that last more than a week or worsen over time.
- Blood in Vomit or Stools: Indicates a more serious condition and should be evaluated by a healthcare provider.
- High-Risk Groups: Children under five, the elderly, or individuals with chronic illnesses should be monitored closely and may need medical evaluation earlier.
6. Preventive Measures
Good Hygiene:
- Handwashing: Wash hands thoroughly with soap and water, especially after using the restroom and before eating.
- Food Safety: Ensure that food is cooked to appropriate temperatures and stored properly. Avoid consuming raw or undercooked foods.
Vaccination:
- Rotavirus Vaccine: For infants, this vaccine can prevent severe gastroenteritis caused by Rotavirus.
Travel Precautions:
- Safe Drinking Water: Be cautious with water quality when traveling. Stick to bottled or properly treated water.
Dietary Management :
Acute gastroenteritis, characterized by inflammation of the stomach and intestines, can cause a range of uncomfortable symptoms such as diarrhea, vomiting, and abdominal pain. One of the key aspects of recovery is managing your diet effectively. Proper dietary choices can help soothe symptoms, prevent dehydration, and speed up recovery. Here’s a guide to navigating your diet during an episode of acute gastroenteritis.
Initial Phase: Rest and Rehydration
- Stay Hydrated: The primary concern during acute gastroenteritis is dehydration due to fluid loss from vomiting and diarrhea. Begin with clear fluids such as:
- Oral Rehydration Solutions (ORS): These contain electrolytes and are specifically designed to replace lost fluids and minerals.
- Clear Broths: Chicken or vegetable broth can provide hydration and some nutrients.
- Diluted Juices: Apple or pear juice, diluted with water, can offer a mild source of hydration and calories.
- Herbal Teas: Ginger or peppermint tea can be soothing and help reduce nausea.
- Avoid:
- Caffeinated Drinks: Coffee, tea, and energy drinks can exacerbate dehydration.
- Alcohol: Can irritate the gastrointestinal tract and worsen dehydration.
- Sugary Drinks: Sodas and fruit juices high in sugar can lead to diarrhea and are not ideal for rehydration.
Transition Phase: Introducing Solid Foods
Once vomiting has subsided and you can keep fluids down, gradually introduce bland, easy-to-digest foods. Follow the BRAT diet as a starting point:
- Bland Foods:
- Bananas: Easy on the stomach and rich in potassium, which helps replace lost electrolytes.
- Rice: Plain white rice is gentle on the stomach and helps firm up stools.
- Applesauce: Provides some nutrients and is easy to digest.
- Toast: Plain toast can help settle the stomach and provide some carbohydrates.
- Other Suitable Foods:
- Plain Crackers: Simple and easy on the stomach.
- Boiled Potatoes: Without skin, as they are bland and low in fiber.
- Cooked Carrots: Soft, well-cooked carrots can be a good source of vitamins without being harsh on the digestive system.
Gradual Reintroduction of Normal Foods
As you start feeling better, gradually reintroduce more diverse foods. Keep these guidelines in mind:
- Choose Low-Fiber Foods: Fiber can be hard to digest when your gut is inflamed. Opt for white rice, plain pasta, and low-fiber vegetables.
- Lean Proteins: Skinless chicken, turkey, or tofu can provide essential nutrients and proteins without being too heavy.
- Cooked Vegetables: Soft, well-cooked vegetables like spinach or squash are easier to digest.
- Hydration Continuation: Continue drinking fluids, including water, herbal teas, and electrolyte solutions, to stay hydrated.
Foods and Drinks to Avoid
- Dairy Products: Milk, cheese, and yogurt can be difficult to digest and may exacerbate diarrhea, particularly if you’re lactose intolerant.
- Fatty Foods: Fried foods, rich sauces, and fatty cuts of meat can irritate the stomach and delay recovery.
- Spicy Foods: Can exacerbate gastrointestinal irritation and should be avoided until you are fully recovered.
- High-Sugar Foods: Sugary snacks and desserts can lead to increased diarrhea and should be avoided during recovery.
- Whole Grains: High-fiber grains like whole wheat bread and bran cereals can be harsh on an inflamed gut and are best avoided until symptoms improve.
Sample Meal Plan for Acute Gastroenteritis
Day 1:
- Breakfast: Clear broth or herbal tea.
- Lunch: ORS or diluted apple juice.
- Dinner: Plain rice or toast with a small amount of applesauce.
Day 2:
- Breakfast: A banana and plain crackers.
- Lunch: Boiled potatoes with a bit of broth.
- Dinner: Plain toast and cooked carrots.
Day 3:
- Breakfast: Plain rice with a small portion of cooked chicken.
- Lunch: Applesauce and plain pasta.
- Dinner: Soft-cooked vegetables and a small serving of lean protein.
Prevention
Preventing acute gastroenteritis involves a combination of good hygiene practices and safe food handling:
- Hand hygiene: Wash hands thoroughly with soap and water, especially before eating and after using the toilet.
- Food safety: Cook food to the proper temperature and avoid consuming raw or undercooked meat. Be careful with dairy products and make sure they are properly refrigerated.
- Water safety: Drink safe, clean water and be cautious when traveling in areas with questionable water quality.
- Vaccination: For rotavirus, a vaccine is available and recommended for infants, which can significantly reduce the risk of severe gastroenteritis.
When to seek medical help
Although most cases of acute gastroenteritis are mild, it is important to seek medical help if:
- Symptoms are severe or persist for more than a few days.
- There are signs of dehydration, such as dry mouth, excessive thirst, or reduced urine output.
- Blood is present in the vomit or stool.
- The symptoms are particularly severe in young children, the elderly, or individuals with weakened immune systems.
Conclusion
Acute gastroenteritis is a common condition that, despite often being unpleasant, can usually be managed with proper care and preventive measures. By understanding the causes, symptoms, and treatment options, you can better prepare yourself and your family to deal with this condition effectively. Always remember that maintaining good hygiene and safe food practices are the keys to reducing the risk of gastroenteritis and staying healthy.