Introduction
Diabetes mellitus type 2, often referred to as type 2 diabetes, is a chronic condition that affects the way the body processes blood sugar (glucose). It is the most common form of diabetes, accounting for about 90-95% of all diabetes cases. This blog aims to provide a detailed overview of type 2 diabetes, including its causes, symptoms, complications, and management strategies.
What Is Type 2 Diabetes ?
Type 2 diabetes occurs when the body becomes resistant to insulin or when the pancreas is unable to produce enough insulin. Insulin is a hormone that helps glucose enter cells to be used for energy. When insulin function is impaired, glucose accumulates in the blood, leading to high blood sugar levels.
Causes And Risk Factors
Several factors contribute to the development of type 2 diabetes, including:
Genetics: A family history of diabetes increases the risk. Lifestyle factors: Poor diet, lack of physical activity, and obesity are important contributors.
Age: Risk increases with age, especially after 45.
Ethnicity: Certain ethnic groups, such as African Americans, Hispanics, Native Americans, and Asians, are at higher risk.
Other medical conditions: Conditions such as high blood pressure and high cholesterol are often associated with type 2 diabetes.
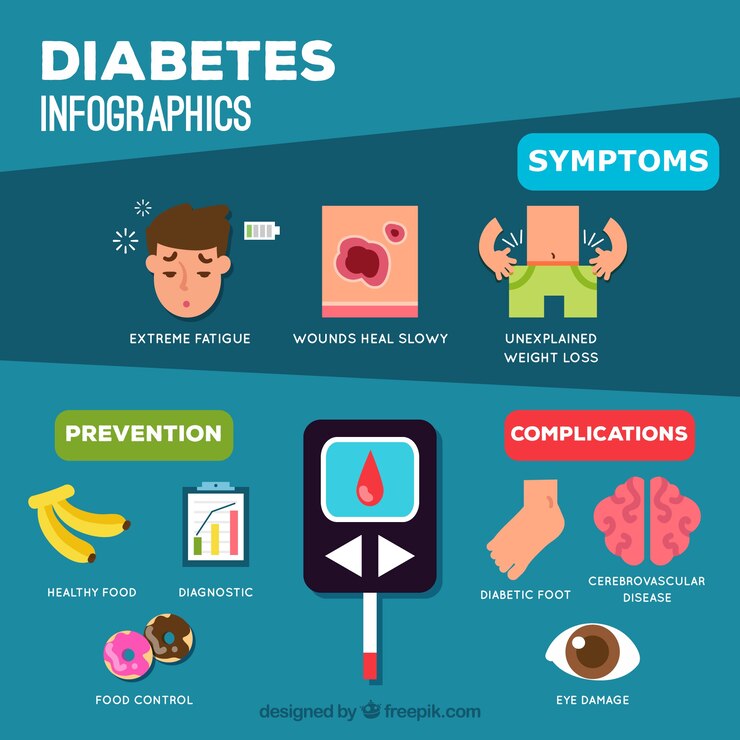
Symptoms
Type 2 diabetes can develop gradually, and symptoms may be mild initially. Common symptoms include:
Increased thirst and frequent urination
Excessive hunger
Unexplained weight loss
Fatigue
Blurred vision
Slowly healing wounds
Frequent infections
Complications
If not properly managed, type 2 diabetes can lead to serious health complications, such as:
Heart disease: Increased risk of heart attack and stroke.
Neuropathy: Nerve damage, especially in the feet.
Nephropathy: Kidney damage, which can lead to kidney failure.
Retinopathy: Eye damage that can lead to blindness.
Foot problems: Poor blood flow and nerve damage can lead to foot ulcers and infections
Effective Treatment On Diabetes Mellitus Type 2
Lifestyle Changes
- Healthy eating
Balanced diet: Focus on a diet rich in vegetables, fruits, whole grains, and lean proteins. Limit processed foods, refined sugars, and unhealthy fats.
Carbohydrate counting: Monitor carbohydrate intake to effectively manage blood sugar levels.
Portion control: Maintain proper portion sizes to manage weight and blood sugar levels.
- Regular physical activity
Aerobic exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise (e.g., walking, cycling, swimming) per week.
Strength training: Include muscle-strengthening activities at least twice a week to improve insulin sensitivity.
Daily activity: Incorporate physical activity into your daily routine, such as climbing stairs or walking short distances.
- Weight management
Achieving a healthy weight: Losing even a little weight (5–10% of body weight) can significantly improve blood sugar control.
Permanent weight loss: Focus on gradual, sustainable weight loss through a combination of diet and exercise.
Medications
There are several medications available to help manage blood sugar levels in type 2 diabetes. These include:
- Oral medications
Metformin: Often the first-line treatment, it reduces glucose production in the liver and improves insulin sensitivity.
Sulfonylureas: These stimulate the pancreas to produce more insulin.
DPP-4 inhibitors: They help lower blood sugar levels without causing weight gain.
SGLT2 inhibitors: These help the kidneys remove glucose from the bloodstream.
Thiazolidine diuretics: They improve insulin sensitivity but may have side effects such as weight gain and increased heart disease risk.
- Injectable medications
GLP-1 receptor agonists: These increase insulin secretion, suppress glucagon release, and slow gastric emptying to reduce blood sugar levels.
Insulin therapy: Necessary for some individuals, especially if other medications are inadequate. Types include long-acting (basal) and rapid-acting (bolus) insulins.
- Blood sugar monitoring
Self-monitoring: Check blood sugar levels regularly using a glucometer. This helps make informed decisions about diet, exercise, and medication.
Continuous glucose monitoring (CGM): A CGM system provides blood sugar readings and trends in real time, allowing for more accurate management.
- Routine medical checkups
Regular visits: Regular appointments with healthcare providers to monitor blood sugar control and adjust treatment plans.
HbA1C test: This test, conducted every 3 to 6 months, provides an average blood sugar level over the past 2-3 months, helping to assess long-term control.
Checking for complications: Regular checkups for diabetes-related complications, such as eye exams, kidney function tests, and foot exams.
- Stress management and mental health
Stress reduction techniques: Practices such as meditation, yoga, and deep breathing exercises can help manage stress, which can affect blood sugar levels.
Mental health support: Seeking help from counselors or support groups can help manage the emotional aspects of living with diabetes.
Conclusion
Type 2 diabetes, although chronic, is manageable with the right lifestyle adjustments and medical care. By understanding the condition, recognizing early symptoms, and following effective management strategies, individuals can live a healthy life despite the diagnosis. Early detection and active management are crucial to prevent complications and improve quality of life.
For more information and support, consult healthcare professionals and consider joining diabetes education programs or support groups. Managing diabetes is an ongoing journey, but with dedication and the right resources, living well with type 2 diabetes is possible.