➢ Introduction:
Begin with an overview of serum iron studies, a group of laboratory tests used to evaluate iron levels in the blood. Explain the importance of iron in various physiological processes, including oxygen transport, energy metabolism, and DNA synthesis.
➢ Understanding Serum Iron Studies:
Discuss the components of serum iron studies, which typically include measurements of serum iron, total iron-binding capacity (TIBC), transferrin saturation, and ferritin levels. Explain the significance of each parameter in assessing iron status and diagnosing iron-related disorders.
➢ Indications for Serum Iron Studies:
Describe the signs, symptoms, and medical conditions that may prompt healthcare providers to order serum iron studies, including:
• Iron deficiency anemia: Characterized by fatigue, weakness, pale skin, shortness of breath, and other symptoms of anemia.
• Iron overload disorders: Such as hereditary hemochromatosis or secondary iron overload due to chronic transfusions or excessive iron supplementation.
• Monitoring iron therapy: Serum iron studies are used to monitor response to iron supplementation or chelation therapy in patients with iron deficiency or iron overload.
➢ Interpreting Serum Iron Studies:
Explain how to interpret serum iron study results, including normal reference ranges and the significance of elevated or decreased levels of serum iron, TIBC, transferrin saturation, and ferritin. Discuss the importance of considering clinical context and other laboratory tests when interpreting serum iron studies.
➢ Clinical Management Based on Serum Iron Studies:
Outline the treatment and management strategies for conditions associated with abnormal serum iron levels, including:
• Iron deficiency anemia: Oral or intravenous iron supplementation, dietary modifications, and treatment of underlying causes.
• Iron overload disorders: Phlebotomy (blood removal), iron chelation therapy, dietary restrictions, and monitoring for complications such as organ damage.
• Monitoring iron therapy: Adjusting iron supplementation or chelation therapy based on serum iron study results and clinical response.
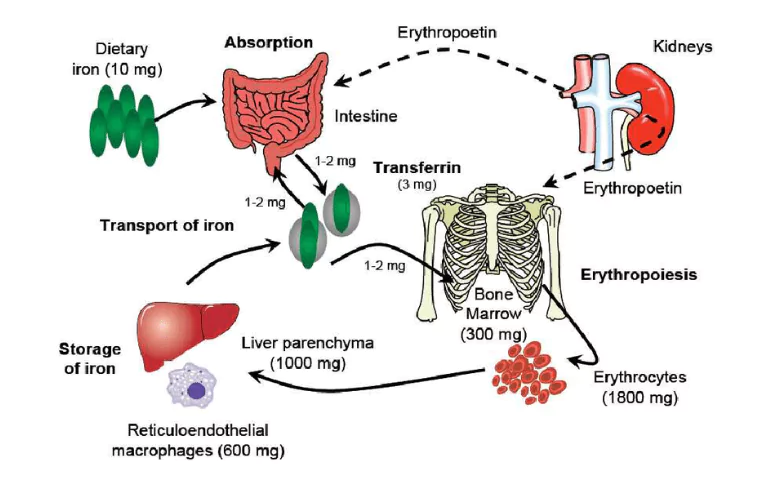
Serum iron studies typically include several parameters that collectively provide insight into an individual’s iron status. These parameters commonly include:
• Serum Iron (SI): This measures the concentration of iron in the blood serum. It reflects the amount of iron circulating in the bloodstream, available for use by the body’s tissues.
• Total Iron-Binding Capacity (TIBC): TIBC measures the maximum amount of iron that can be bound by transferrin, a protein that transports iron in the blood. It indirectly assesses the body’s capacity to bind and transport iron.
• Transferrin Saturation (TSAT): TSAT represents the percentage of transferrin binding sites that are occupied by iron. It is calculated as the ratio of serum iron to TIBC, multiplied by 100. TSAT provides an indication of the proportion of available transferrin-bound iron relative to the total binding capacity.
• Ferritin: Ferritin is a protein that stores iron in cells, primarily in the liver, spleen, and bone marrow. Serum ferritin levels reflect the body’s iron stores. Low ferritin levels are suggestive of iron deficiency, while elevated levels may indicate iron overload or inflammation.
• Transferrin: While not always included in routine serum iron studies, transferrin levels may be measured to assess the body’s iron transport capacity. Transferrin is the primary protein responsible for transporting iron in the bloodstream.
These parameters collectively provide valuable information about an individual’s iron status, including iron deficiency, iron overload, or normal iron metabolism. Interpreting these parameters in conjunction with clinical context and other laboratory tests allows healthcare providers to diagnose and manage iron-related disorders effectively.