Introduction
Preeclampsia is a pregnancy complication that features high blood pressure and symptoms of damage to other organs, most often the liver and kidneys. It usually begins after 20 weeks of pregnancy in women whose blood pressure was previously normal. If left untreated, preeclampsia can lead to serious — even fatal — complications for both mother and baby.
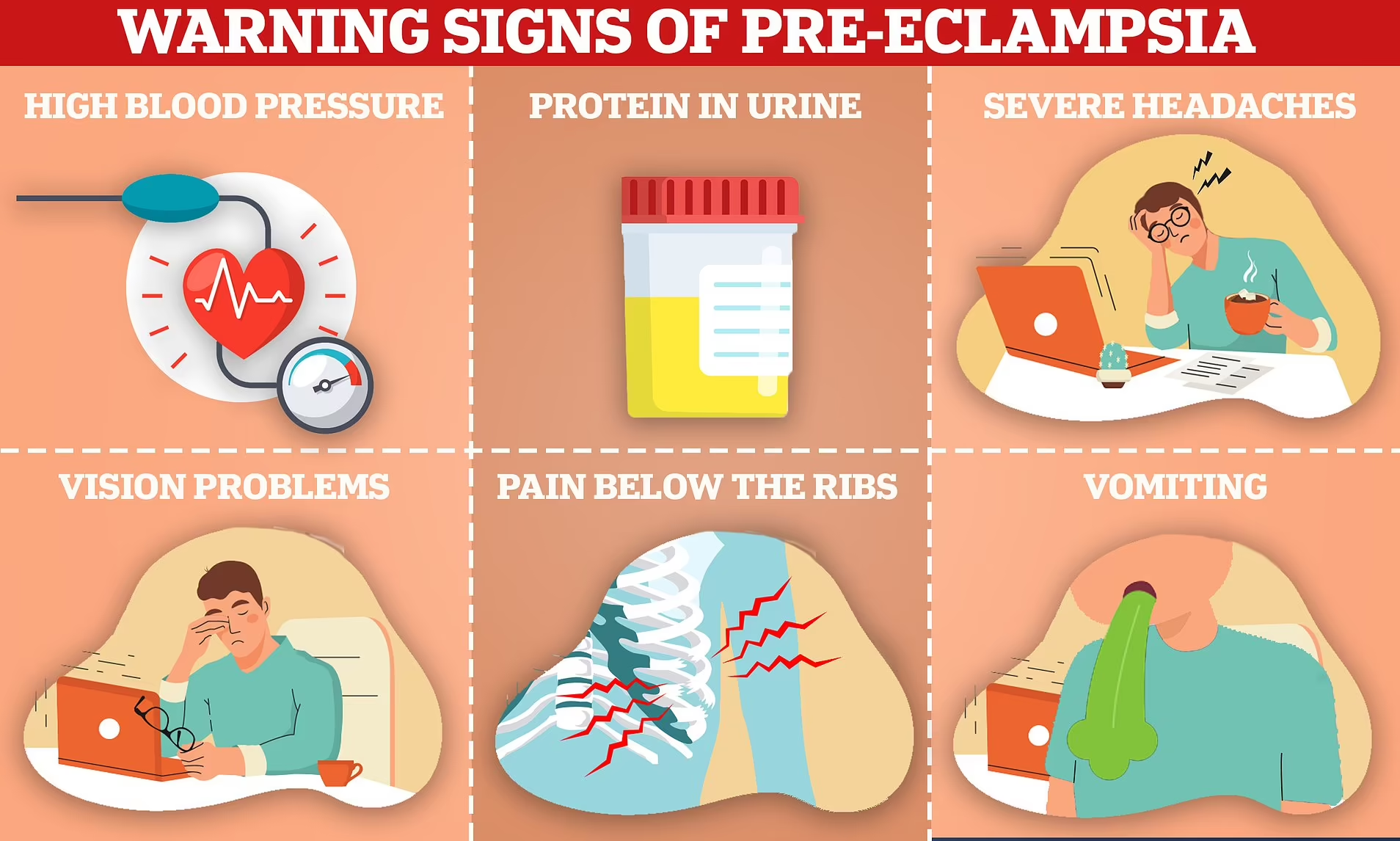
Symptoms And Diagnosis
The symptoms of preeclampsia can vary widely and may include:
- High blood pressure (140/90 mm Hg or higher)
- Excess protein in the urine (proteinuria)
- Severe headache
- Vision changes, including temporary loss of vision, blurred vision or sensitivity to light
- Pain in the upper abdomen, usually on the right side just below the ribs
- Nausea or vomiting
- Decreased urine output
- Shortness of breath due to fluid in the lungs
The diagnosis is usually made based on these symptoms as well as a routine prenatal checkup. Blood tests, urine analysis, and ultrasounds may be performed to confirm the condition and assess its severity.
Risk Factors
While the exact cause of preeclampsia is unknown, several risk factors have been identified:
- First-time pregnancy
- History of preeclampsia in previous pregnancies
- Family history of preeclampsia
- Obesity
- Multiple pregnancies (twins, triplets, etc.)
- Maternal age (over 35 or under 20)
- Certain conditions, such as chronic hypertension, diabetes, kidney disease, and autoimmune disorders
Potential Complications
Preeclampsia can have serious consequences for both mother and baby if not managed properly. Some potential complications include:
- Eclampsia: This serious condition can cause seizures in the mother.
- HELLP syndrome: A severe form of preeclampsia, characterized by hemolysis, elevated liver enzymes, and low platelet count.
- Fetal growth restriction: Preeclampsia can affect the arteries carrying blood to the placenta, thereby limiting fetal growth.
- Premature birth: Often, premature delivery is necessary to prevent life-threatening complications.
- Placental abruption: The placenta may separate from the inner wall of the uterus before delivery, which can be life-threatening for both mother and baby.
Treatment
Preeclampsia is a serious pregnancy complication that requires careful management to ensure the health and safety of both the mother and the baby. The primary treatment for preeclampsia is the delivery of the baby, as the condition typically resolves once the placenta is removed. However, the timing of delivery and the specific treatments used can vary depending on the severity of the condition and the gestational age of the fetus.
Initial Management
Monitoring and Assessment
- Blood Pressure Monitoring: Regular monitoring of blood pressure to track the severity of hypertension.
- Urine Tests: Frequent checks for proteinuria to assess kidney function.
- Blood Tests: To monitor liver function, platelet count, and the presence of other markers that indicate the severity of preeclampsia.
- Fetal Monitoring: Ultrasounds and non-stress tests to check the baby’s growth and well-being.
Lifestyle Adjustments
- Bed Rest: In some cases, partial or complete bed rest may be recommended, although this practice is becoming less common due to potential complications from prolonged inactivity.
- Dietary Changes: While no specific diet can prevent or treat preeclampsia, maintaining a balanced and nutritious diet is essential for overall health.
Medical Treatments
Antihypertensive Medications
- Medications like labetalol, nifedipine, and methyldopa are commonly used to lower blood pressure and reduce the risk of complications. The choice of medication depends on the severity of hypertension and the patient’s overall health.
Corticosteroids
- If the pregnancy is between 24 and 34 weeks, corticosteroids may be administered to accelerate fetal lung development in case early delivery becomes necessary.
Magnesium Sulfate
- This medication is often used to prevent seizures (eclampsia) in women with severe preeclampsia. It may be administered intravenously during labor and for 24 hours after delivery.
Other Medications
- Depending on the individual case, other medications may be used to manage symptoms and reduce complications. For example, diuretics might be prescribed to manage fluid retention in certain cases.
Hospitalization
In cases of severe preeclampsia, hospitalization may be necessary for closer monitoring and more intensive treatment. Hospital care can include:
Intravenous Medications
- IV medications can be administered to control blood pressure more effectively and manage other symptoms.
Continuous Fetal Monitoring
- Continuous monitoring of the baby’s heart rate and other vital signs to ensure the baby is not in distress.
Immediate Access to Emergency Care
- In the hospital setting, immediate medical intervention is available if the condition worsens or complications arise.
Delivery
The only definitive cure for preeclampsia is the delivery of the baby and the placenta. The timing of delivery depends on the severity of the condition and the health of both mother and baby.
Preterm Delivery
- If preeclampsia is diagnosed before 37 weeks, the healthcare provider will carefully weigh the risks of preterm delivery against the risks of continuing the pregnancy. In some cases, early delivery may be necessary to protect the health of the mother and baby.
Term Delivery
- If the pregnancy is at 37 weeks or beyond, delivery is usually recommended to prevent further complications.
Cesarean Section
- A C-section may be required if the mother’s or baby’s health is at significant risk, or if the baby is not in a position suitable for vaginal delivery.
Postpartum Care
Preeclampsia can persist or even develop after delivery (postpartum preeclampsia), so careful monitoring continues after birth. Postpartum care includes:
Continued Monitoring
- Blood pressure and overall health are monitored for several weeks postpartum to ensure the condition is resolving.
Medications
- Antihypertensive medications may be continued postpartum until blood pressure stabilizes.
Support and Education
- Providing the mother with education about the signs and symptoms of postpartum preeclampsia and ensuring she has support and resources available.
Prevention
While there is no sure way to prevent preeclampsia, certain measures can reduce the risk:
- Regular prenatal care: Early detection through regular check-ups is important.
- Healthy lifestyle: Maintaining a healthy weight, eating a balanced diet and engaging in regular physical activity.
- Management of existing conditions: Proper management of chronic conditions such as hypertension and diabetes.
- Low-dose aspirin: In some cases, low-dose aspirin may be recommended for high-risk women after the first trimester.
Conclusion
Preeclampsia is a serious condition that requires careful monitoring and management to ensure the safety of both mother and baby. Awareness of the symptoms and risk factors, along with regular prenatal care, can help in early detection and effective management of this potentially life-threatening condition. If you suspect you have preeclampsia or are at risk, consult your healthcare provider for proper guidance and care.