Introduction
Rheumatoid Arthritis (RA) is a chronic autoimmune disorder characterized by inflammation and pain in the joints, affecting millions worldwide. Among the diagnostic tools available to clinicians, the RA Factor lab test stands as a crucial marker in the identification and management of this debilitating condition.
Understanding Rheumatoid Arthritis
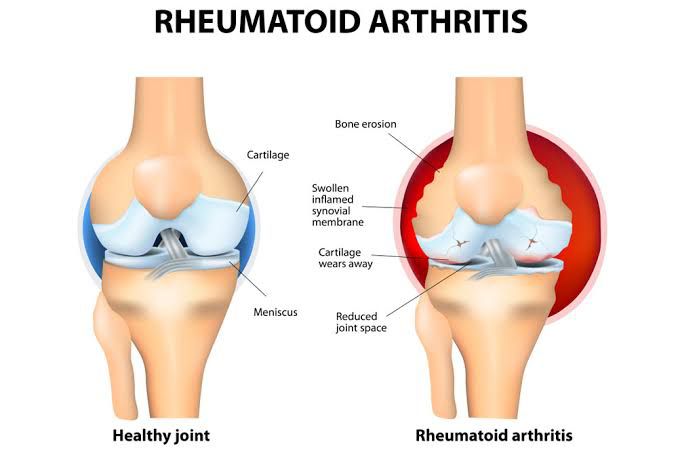
Rheumatoid Arthritis is an autoimmune disease in which the body’s immune system mistakenly attacks its tissues, primarily targeting the synovium—the lining of the joints. This results in inflammation, pain, stiffness, and eventually joint damage and deformity.
Role Of The RA Factor Lab Test
The Rheumatoid Arthritis Factor (RA Factor) lab test is a blood test that detects the presence of autoantibodies called rheumatoid factors in the bloodstream. Rheumatoid factors are antibodies produced by the immune system that mistakenly target healthy tissues, particularly in the joints. While not exclusive to Rheumatoid Arthritis, elevated levels of RA Factor are strongly associated with the disease and play a significant role in its diagnosis.
Indications For RA Factor Testing
The RA Factor lab test may be ordered for individuals presenting with symptoms suggestive of Rheumatoid Arthritis, including joint pain, swelling, stiffness, and fatigue.
Interpreting RA Factor Levels
Interpreting RA Factor levels requires consideration of various factors, including the patient’s clinical presentation, medical history, and other diagnostic tests. While elevated RA Factor levels are indicative of autoimmune activity, not all individuals with RA will test positive for RA Factor. Conversely, some individuals without RA may have elevated RA Factor levels. Therefore, RA Factor testing is just one component of the diagnostic evaluation for Rheumatoid Arthritis.
Clinical Implications And Management
A positive RA Factor test, along with other clinical and laboratory findings, may support a diagnosis of Rheumatoid Arthritis. Early detection allows for prompt initiation of treatment, which may include disease-modifying antirheumatic drugs (DMARDs), nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and biologic agents. Additionally, lifestyle modifications and physical therapy play integral roles in managing RA and improving quality of life for affected individuals.
Symptoms
- Joint Pain: Persistent pain, swelling, and tenderness in multiple joints, especially smaller joints like those in the hands and feet, are characteristic of RA.
- Joint Stiffness: Morning stiffness lasting for at least 30 minutes, or stiffness after prolonged periods of inactivity, is a hallmark symptom of RA.
- Joint Swelling: Swelling or inflammation in the joints, often accompanied by warmth to the touch.
- Fatigue: Profound fatigue or lack of energy, which may interfere with daily activities.
- Generalized Weakness: Weakness or a feeling of general malaise may accompany RA.
- Decreased Range of Motion: Difficulty moving certain joints due to stiffness or pain, leading to a decreased range of motion.
- Fever: Low-grade fever, particularly in the early stages of RA or during disease flares.
- Weight Loss: Unintended weight loss, which can occur as a result of the inflammatory process associated with RA.
- Numbness and Tingling: Sensations of numbness or tingling in the hands and feet, which may be indicative of nerve involvement in RA.
- Symmetrical Joint Involvement: RA often affects joints symmetrically, meaning that if one joint is affected, the corresponding joint on the other side of the body is also affected.
It’s important to note that these symptoms can also be indicative of other conditions, so diagnosis of RA typically involves a comprehensive evaluation by a healthcare provider, including a physical examination, medical history review, and possibly imaging studies or blood tests such as the RA Factor test.